Regarding intraocular foreign bodies (IOFBs), it risks stating the obvious to declare that you can’t remove what you can’t see or don’t know is there. Yet this is exactly the situation for IOFBs until very recently. Because hemorrhage is an almost constant companion to ocular trauma, direct observation of retained IOFBs was (is) essentially impossible. X-ray revolutionized the ability to detect many foreign bodies (FBs), but then localizing the object as intraocular or extraocular remained a challenge. Additionally, many FBs are invisible on X-ray and remained enigmatic. It was not until the dawn of ultrasound and computed tomography (CT) that accurate detection and localization became predictable. Even then, removal of the FB posed different technical challenges; what use is it to know of an IOFB if attempted removal causes more trauma and loss of the eye? Clearly, detection and management had to progress hand-in-hand.
These are challenges that faced deployed military ophthalmologists until surprisingly recently. Although sophisticated surgical techniques for removal became available soon after Vietnam, detection remained rooted in World War I-II techniques. It was not until after Desert Shield/Desert Storm (1990-91) that CT scanners were first deployed to the field, providing significant advancement. Ocular CT is now standard practice in head trauma in the combat zone. This article brings light to that evolution.
Approximately 18-41% of open-globe injuries involve IOFBs, the majority of which are work-related (54-72%), followed by injuries at home (30%).1 Ocular injuries from FBs vary by size, weight, composition, and the anatomic zone of injury. Associated vision loss depends on the amount of damage to intraocular structures, the presence of retinal detachment, and macular injury. The majority of eye injuries with IOFBs occur in young men between 21-40 years of age (66%). The most common causes for IOFBs are hammering (60-80%), power tool use (18-25%), and weapon-related injuries (19%).1 Unlike the non-combat-related eye injuries with foreign bodies seen in the civilian population, combat-related injuries often involve polytrauma; eye injuries themselves tend to represent ocular polytrauma requiring management by multiple ophthalmic subspecialists. In fact, Colyer et al.2 reported that 79 eyes of 70 U.S. Service members (25%) evaluated at the former Walter Reed Army Medical Center (WRAMC) for combat-related ocular injury between 2003 and 2007 had an IOFB. Ocular trauma associated with IOFBs often carries a poor prognosis; extensive intraocular injury due to IOFBs has been reported to significantly affect post-operative visual acuity.2 The presence of IOFBs in open-globe injuries also increases the risk of post-traumatic endophthalmitis. In a retrospective case series, Banker et al.3 observed that the rate of culture-positive endophthalmitis after open-globe repair was 8.1% in eyes with IOFBs vs.1.6% in eyes without IOFBs (P < 0.01).
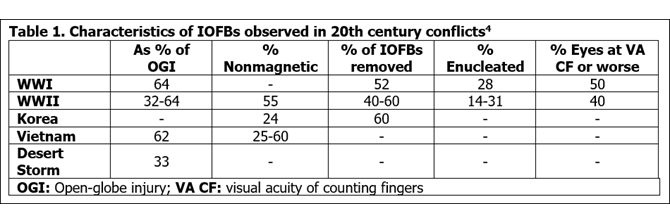
The diagnosis and management of IOFBs in both civilian and military personnel have been challenges to ophthalmologists for at least two centuries. Over the years, management of open-globe injuries with and without FBs has dramatically improved. This has been driven by the challenging combat-related ocular injuries managed by military ophthalmologists who have the responsibility of providing the highest quality care to injured Service members. This article provides an overview of the evolution of diagnostic and therapeutic techniques for the detection of IOFBs over the past century and the contributions military ophthalmologists have made to this evolution. The diverse nature of IOFBs as well as their variability in size, impact site, and resultant intraocular damage makes meaningful comparisons of statistics difficult; however, some observations are possible (Table 1).
Evolution of IOFB Detection Methods
Military physicians were quick to employ radiographic methods after Wilhelm Röntgen developed the X-ray in 1895 and demonstrated its value in medicine.5 Only six months after this discovery, Lieutenant Colonel Giuseppe Alvaro of the Italian Army made radiographs to find bullets in the forearms of two soldiers in the Abyssinian War of 1896. X-ray technology provided a precise method of detecting retained FBs, and in many cases, eliminated the need for inappropriate exploration of the wound. General radiography was employed to good effect in the subsequent Graeco-Turkish War of 1897, the Tirah Campaign of 1897, the River War of 1898, and the Boer and Spanish-American Wars of 1899.5 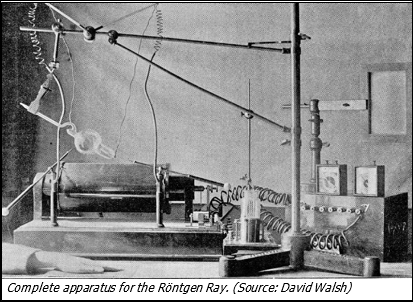
The value of X-ray technology in civilian ophthalmology was also quickly recognized and adopted. In 1896, two American ophthalmologists (Charles H. Williams and his brother Francis H. Williams) detected a metallic IOFB in a boy who had sustained it by hammering on a cartridge. After 10 minutes of exposing the patient to X-ray, they had localized and successfully removed a strip of copper from the vitreous.6
A large number of X-ray techniques for IOFB detection had been developed by the outbreak of World War I. William Sweet, who had developed the Sweet localizer for metallic IOFBs in 1897 and an improved version in 1909, treated injured U.S. Army soldiers during World War I by using these methods.6 Sir James Mackenzie Davidson, a British ophthalmologist, devised the cross-thread method of localization and applied stereoscopy to the viewing of radiographs. 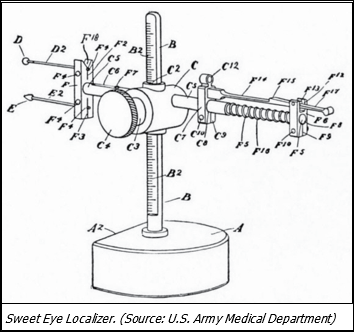 He published his work in 1916 while providing care for World War I casualties. Sweet's method of IOFB localization, along with other methods of localization by simple radiographs focused at cross measurements, stereoscopic radiographs, and fluoroscopy, were employed during World War I.7 At the beginning of World War I, European armies were provided standard gas X-ray tubes; however, more powerful radiographic equipment was introduced as the war progressed. This advanced equipment was supplied to the American Expeditionary Force during the war, which made full use of these technologies in the detection of FBs.5 Despite the advances in X-ray techniques, it appeared that the British Army preferred to use giant magnets to detect magnetic FBs.5
He published his work in 1916 while providing care for World War I casualties. Sweet's method of IOFB localization, along with other methods of localization by simple radiographs focused at cross measurements, stereoscopic radiographs, and fluoroscopy, were employed during World War I.7 At the beginning of World War I, European armies were provided standard gas X-ray tubes; however, more powerful radiographic equipment was introduced as the war progressed. This advanced equipment was supplied to the American Expeditionary Force during the war, which made full use of these technologies in the detection of FBs.5 Despite the advances in X-ray techniques, it appeared that the British Army preferred to use giant magnets to detect magnetic FBs.5
The British Army stated that X-ray examination and localization in austere conditions was nearly impossible, and that all suspected cases of IOFBs should be evaluated via the magnet test.8Giant magnets were made available at Boulogne, Étaples, and Rouen, which were three of the large “eye centers” that were set up at bases by the British. The magnet test was described as “the simplest and most efficient one for detection of a magnetic foreign body in the eye.” 8 Cases of IOFBs were common during the war, therefore these magnets were used frequently. On a typical day, 4-5 cases, and sometimes as many as 15 cases, were put up to the magnet in the suspicion of an IOFB. All eye centers needed access to such magnets because of the high number of casualties with IOFBs; however, the magnets were too bulky and expensive to meet this need. To resolve this issue, a “mobile magnet” was developed, which involved a giant magnet mounted to an ambulance that could be transported as needed. This method, however, was also impractical due to the heavy weight of the magnet and the subsequent challenge of transporting it over long distances on poorly built roads. Shortly thereafter, one of the U.S. base hospitals was equipped with a smaller, but very powerful magnet, which was 15 inches long, weighed 30 pounds, and cost approximately $70 in 1918. This magnet made it possible to equip all base hospitals with magnets that are powerful, yet practical for IOFB detection.8 During the remaining years of the 20thcentury, a standard FB X-ray series for suspected IOFBs was developed incorporating Waters', Caldwell, and lateral views. Metal locators (Berman, Roper-Hall, and Bronson-Turner) were developed and ultrasonography also became widely available; however, significant advances in our ability to detect IOFBs had to await the advent of CT in the 1970s, and later, magnetic resonance imaging (MRI) for non-metallic FBs.5
Despite the advances in X-ray techniques, it appeared that the British Army preferred to use giant magnets to detect magnetic FBs during World War I.
Management of IOFBs: World War I to Present
World War I and Interwar Period
Julius Hirschberg revolutionized the treatment of IOFBs by being the first to apply an electromagnet for their extraction.6 Extraction employing giant and/or hand-held magnets was common by either the anterior route (whereby a magnetic FB in the posterior segment was brought by the magnet into the anterior chamber and removed through a corneal incision) or by the posterior route, usually via direct incision through the sclera, choroid or, if attached, retina, based on proximity to the FB.
While use of a magnet for IOFB removal was a significant advancement, IOFB removal still posed many challenges. On occasion, a magnet would be used to identify the magnetic nature of an IOFB, with the casualty experiencing pain from the FB's movement. Shoemaker6 recommended that, if practical, IOFB removal should take place as soon after injury as possible while attempting to minimize additional damage to the eye, but added that “…removal by forceps from the vitreous can scarcely be considered as practical, because when successful, it is more a question of luck than skill. If large enough to get, we might as well take the eyeball." Additional challenges in the removal of IOFBs were illustrated by de Schweinitz and Greenwood9 who added that, while moderate-sized IOFBs (i.e., 4 x 2 mm) may be removed by a magnet or other method, the result was typically a blinded eye. However, smaller FBs (i.e., 2 x ½ mm) were often easier to remove and had significantly better visual outcomes.9
Extraction of an FB by the posterior route often led to poor visual outcomes. In a series of 48 patients who underwent IOFB extraction by the posterior route, 31% were blinded, 40% had light perception or counting fingers (CF) vision, 15% had "useful vision" (3/60-6/12), and 15% had "good vision" (6/9 or 6/6) after the procedure.6 In some cases of extraction through the posterior route, it was possible to watch forceps move in the vitreous with an ophthalmoscope. After one successful extraction, it was noted that "the lens remained clear, but the retina was largely detached by proliferative chorioretinitis [proliferative vitreoretinopathy (PVR)], traumatic."7 At that time, retinal detachment was considered untreatable. It would take almost another 100 years for modern retina surgery and instrumentation to develop. Although retinal holes were first noted after the development of the ophthalmoscope, their significance in the development of retinal detachment was only recognized in 1918 by Jules Gonin. He successfully treated several cases by cauterizing the sclera in the area of the retinal tear.6
World War II
Combat circumstances in World War II contributed to poor detection and management of IOFBs, which were frequent due to the increased use of explosive devices. At the early points in their care, Service members with IOFBs were rarely evaluated by an ophthalmologist, resulting in delayed treatment of ocular injuries. In addition, most FBs were the result of fragments generated by explosives (particularly landmines) and were typically not magnetic. Removal of these FBs was difficult, if not impossible, and often caused additional damage to the structures of the eye.10 The controversy over the advisability of anterior versus posterior route extraction of magnetic FBs continued; meanwhile Verhoeff's pars plana vitrectomy approach, the Thorpe endoscope, and the Berman locator were employed. PVR was again recognized as a serious problem. Wilder, at the then Army Institute of Pathology, studied the FBs removed from 150 enucleated eyes, 89 of which were non-magnetic.10 The authors of Surgery in World War II, Ophthalmology and Otolaryngology concluded: "Since, at best, the results of treatment of IOFBs are not outstanding, no precaution should be overlooked that can improve them."10
Additional innovation during the World War II era was Ridley’s epochal development of the intraocular lens following his observations in war casualties:
“Ridley drew on prior observations as a military surgeon that both glass and acrylic, under certain conditions, appeared to be inert within body tissues. During World War II some airplane cockpit and gunnery canopies were fabricated from glass and PMMA [polymethyl methacrylate (i.e., PlexiglasTM)]. When a canopy was shattered by gunfire, fragments of this material sometimes penetrated the eyes of the flight crew. Ridley observed that unless a sharp edge of the plastic material rests in contact with a sensitive and mobile portion of the eye, the tissue reaction is insignificant. This observation has become one of the most important principles now universally applied to modern lens design and implantation.”11
Early in the 20th century, a number of contact lens devices were developed to assist with IOFB detection, such as the Comberg technique, which employed a modified Zeiss lens bearing four radiopaque markers.6
Korean War
The prevalence of significant eye injuries in U.S. personnel was reported as being between 3 and 8% during the Korean War. Twenty-four percent of FBs found in 129 eyes were non-magnetic; FBs were removed in 60% of the 129 eyes. As had been true in the World Wars, artillery and tank shell fragments produced most of the eye injuries.4 Noting the protection provided by even an ordinary pair of glasses, Fair12 proposed the use of what he termed “Eye Armor” consisting of case-hardened lenses and metal side shields, to protect Service members. Unfortunately, they were rejected, in part because of visual field restriction.
Vietnam War
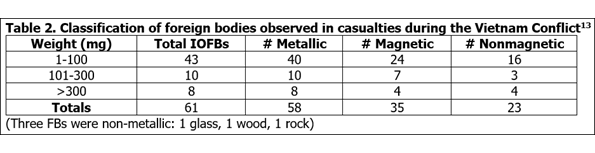
IOFBs continued to be a major problem over the years of the war, in part because no acceptable form of eye protection was provided to ground combatants. In an analysis of ocular and ocular adnexal injuries sustained by U.S. forces, 272 were noted to contain IOFBs, comprising 15% of the ocular injuries.13 A separate analysis of 100 eye injuries in 57 casualties cared for at WRAMC identified 22 IOFBs. An analysis conducted at Fitzsimons Army Hospital found retained IOFBs in 51 of 281 casualties. Evaluation of wound data and munitions effectiveness analysis demonstrated that 68% of non-fatal war wounds of all types in the war were the result of fragments from munitions.13,14 Sponaugle and McKinley studied 61 FBs removed from the eyes, orbital, or adnexal soft tissues of soldiers and Marines between 1968 and 1969; relevant results are in Table 2.13
Extraction of magnetic posterior segment IOFBs by the anterior route gave way to 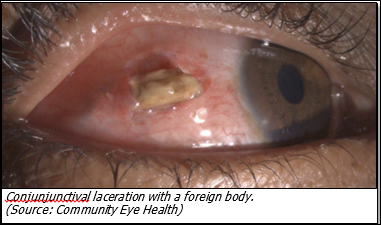 extraction through a scleral incision using a Bronson magnet after diathermy was applied to the choroid. On occasion, the FB would cut through the retina (if attached) and the choroid. If not, the FB would be removed through a choroidal incision when it bulged in response to the magnetic force. Sweet's and Comberg's localization methods were employed when available, and a modified spectacle frame was used when they were not. Penner and Passmore15 described a magnet-ultra sound test. Cowden and Runyan16 compared ultrasonography and radiography in FB detection.
extraction through a scleral incision using a Bronson magnet after diathermy was applied to the choroid. On occasion, the FB would cut through the retina (if attached) and the choroid. If not, the FB would be removed through a choroidal incision when it bulged in response to the magnetic force. Sweet's and Comberg's localization methods were employed when available, and a modified spectacle frame was used when they were not. Penner and Passmore15 described a magnet-ultra sound test. Cowden and Runyan16 compared ultrasonography and radiography in FB detection.
Major advances were made in our understanding of FB injuries and their appropriate management in the 1970s. CT and, later MRI; closed eye vitrectomy with modern instrumentation; therapeutic modalities such as endolaser, silicone oil, and other fluids; combined with a better understanding of PVR and its management; and the management of IOFBs by trained retinal surgeons have resulted in improvements in visual acuity and globe retention. In light of these advances, the best visual results for combat-injured Service members with open-globe injuries and IOFBs can only be achieved when these injuries are managed by subspecialty-trained vitreoretinal specialists at a Level 4 or 5 facility or similar facility where modern instrumentation and equipment for retinal surgery is available.17
Operations Iraqi and Enduring Freedom
Significant advances in the ability to manage IOFBs have been made in the past two decades. MRI (in the absence of magnetic FBs) has allowed improved visualization of non-magnetic and nonmetallic IOFBs. This imaging technique has also improved our understanding of the role the vitreous plays in the development of PVR and has improved our understanding of the optimal time for IOFB extraction. IOFBs are being managed by vitreoretinal subspecialists in Level 5 Military Treatment Facilities (MTFs). Surgical instrumentation for retinal surgery has been miniaturized, thus decreasing the possibility of intraoperative injury. Ancillary therapeutic modalities and the widespread use of topical and systemic fluoroquinolone antibiotics has reduced the incidence of endophthalmitis. As previously mentioned, Colyer et al.2 reported on 79 eyes containing IOFBs in 70 U.S. soldiers treated at WRAMC with a follow-up at 6 months. Their treatment encompassed a 20-gauge, 3-port vitrectomy with IOFB removal through a limbal or a pars plana incision. The IOFBs varied from 0.1-20 mm (mean = 3.7 mm). The median time to removal was 21 days. The average pre-operative vision was 20/400; the average post-operative vision was 20/120. A visual acuity of 20/40 or better was achieved in 53.4% of casualties and 20/200 or better in 77.5%. There were no cases of endophthalmitis, siderosis, or sympathetic uveitis. However, 10.3% of the casualties either became blind or required enucleation in 6 months. Not surprisingly, poor visual outcome correlated with extensive intraocular injury, as did the prevalence of PVR (21%).
Conclusions
The past century has seen dramatic improvement in the diagnosis and management of war-induced IOFBs. Nonetheless, the paramount importance of preventing such injuries from occurring remains. Efforts must continue to develop and distribute improved forms of eye protection, which will especially provide increased protection from blast effects. 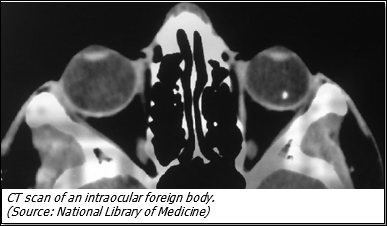 Despite the favorable results obtained from delayed removal of IOFBs, at least one posterior segment subspecialist should be a member of the Eye Team component of the Head and Neck Team at a Level 3 deployed MTF. This is particularly beneficial in cases where IOFBs necessitate immediate removal (e.g., pure copper FBs), and the United States may not continue to enjoy the level of air superiority necessary to permit evacuation from the war zone, thus requiring prolonged field care. Additionally, U.S. military medical personnel are required to provide humanitarian care for host country nationals who present with IOFBs and cannot be evacuated to higher levels of care. IOFBs are a common occurrence in war and may be multiple, with one FB potentially masking another; this necessitates repeating the CT scan after initial treatment in military casualties. For radiolucent FBs not visible by either CT or MRI, ocular ultrasound by a trained ocular ultrasonographer can be used after any open globe has been surgically repaired.
Despite the favorable results obtained from delayed removal of IOFBs, at least one posterior segment subspecialist should be a member of the Eye Team component of the Head and Neck Team at a Level 3 deployed MTF. This is particularly beneficial in cases where IOFBs necessitate immediate removal (e.g., pure copper FBs), and the United States may not continue to enjoy the level of air superiority necessary to permit evacuation from the war zone, thus requiring prolonged field care. Additionally, U.S. military medical personnel are required to provide humanitarian care for host country nationals who present with IOFBs and cannot be evacuated to higher levels of care. IOFBs are a common occurrence in war and may be multiple, with one FB potentially masking another; this necessitates repeating the CT scan after initial treatment in military casualties. For radiolucent FBs not visible by either CT or MRI, ocular ultrasound by a trained ocular ultrasonographer can be used after any open globe has been surgically repaired.
The Vision Center of Excellence (VCE) fact sheet titled “Handling of Ocular and Adnexal Foreign Bodies Removed at DoD and VA Medical Facilities” provides valuable information regarding the submission and analysis of FBs by the Joint Pathology Center (JPC) after removal. Another VCE fact sheet, “Detection and Initial Management of Ocular Foreign Bodies and Injuries,” is in development and will provide general principles for deployed ophthalmologists on the initial diagnosis and treatment of IOFBs
References
- Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: A review. Surv Ophthalmol. 2016;61(5):582-596.
- Colyer MH, Weber ED, Weichel ED, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology. 2007;114(8):1439-1447.
- Banker TP, McClellan AJ, Wilson BD, et al. Culture-positive endophthalmitis after open-globe injuries with and without retained intraocular foreign bodies. Ophthalmic Surg Lasers Imaging Retina. 2017;48(8):632-637.
- Wong TY, Seet MB, Ang CL. Eye injuries in twentieth century warfare: a historical perspective. Surv Ophthalmol. 1997;41(6):433-459.
- Thomas AM. The first 50 years of military radiology 1895-1945. Eur J Radiol. 2007;63(2):214-219.
- Duke-Elder WS, Wybar KC, Cook C. System of Ophthalmology. Injuries: Mechanical Injuries. Vol. 14, Part 1; 1972.
- Lynch C, Weed FW, McAfee L. The Medical Department of the United States Army in the World War. 1923; Available at: http://history.amedd. army.mil/books.html. Accessed December 21, 2017.
- Greenwood A. Ophthalmology in the American Expeditionary Forces. In: Ireland MW, ed. Medical Department of the US Army in World War I. Vol 11, Part 2. Washington DC: War Department, US Government Printing Office; 1924.
- de Schweinitz GE, Greenwood AC. Medical Department of the US Army in World War I. Vol 11 Part 2. Washington DC: War Department, US Government Printing Office. 1924.
- Coates JB Jr, Randolph ME, Canfield N, eds. Ophthalmology and Otolaryngology. In: Hays SB, Coates JB Jr, eds. Surgery in World War II. Washington, DC: US Department of the Army, Medical Department, Office of The Surgeon General; 1957.
- Apple DJ, Sims J. Harold Ridley and the invention of the intraocular lens. Surv Ophthalmol. 1996;40(4):279-292.
- Fair JR. Eye armor. Am J Ophthalmol. 1957;43(2):258-264.
- La Piana FG, Hornblass A. Military ophthalmology in the Vietnam War. Doc Ophthalmol. 1997;93(1-2):29-48.
- Evaluation of Wound Data and Munitions Effectiveness in Vietnam. US Departments of the Army, Navy and Air Force, Washington. Vol. 1: D-51.
- Cowden JW, Runyan TE. Localization of intraocular foreign bodies. Further experiences in ultrasonic vs radiologic methods. Arch Ophthalmol. 1969;82(3):299-301.
- Lenhart MK, Savitsky E, Eastbridge B, Eastridge B, United States Department of the Army Office of the Surgeon General. Combat Casualty Care: Lessons Learned from OEF and OIF. Borden Institute, Office of the Surgeon General, Department of the Army; 2012.